This leaflet is to help you understand what Pyloric Atresia is, what tests you need, and the implication of being diagnosed for you and your baby.
What is pyloric atresia?
Normally, food that is swallowed passes through the esophagus into the stomach and then into the duodenum followed by the small intestine (bowel), then the large intestine and the contents which have not been digested pass out through the anus. The connection between the stomach and the duodenum is called the pylorus. Very rarely there is a blockage or obstruction in the outlet of the stomach. This is called pyloric atresia.
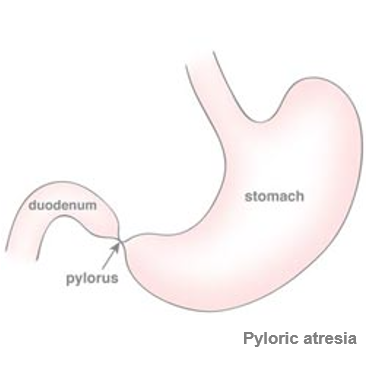
Pyloric atresia
There are three types of pyloric atresia:
• In type I, the most common type, there is a pyloric membrane that completely divides the stomach from the duodenum. This type happens in just over 59% of cases.
• In type II, there is a solid cord in the pylorus between the stomach and the duodenum. This happens in about 1/3 of cases.
• In type III, a gap is present between the stomach and duodenum. This happens in about 9% of cases.
Pyloric atresia is extremely rare and happens in about 1 in 100,000 babies.
How does a pyloric atresia happen?
The exact cause of pyloric atresia is unknown. There are two ways in which a pyloric atresia may develop:
- In Type 1 it is thought that there is a stop in embryological development between the 5th and the 7th week of gestation which causes the problem.
- Type 2 and Type 3 may be the result of an abnormal genetic modification that causes a separation of the intestinal tissue layers and prevents the control of the normal wound healing. An inflammatory reaction then takes place, and a thick scar is formed in the pylorus, causing a blockage in the pathway between the pylorus and the duodenum.
Are there any other problems that a baby with pyloric atresia might have?
Pyloric atresia is commonly isolated, meaning that it is the only problem that the fetus has. However, pyloric atresia may be associated with genetic diseases, in which case, additional abnormalities may be present.
Pyloric atresia may be seen in babies who have a very rare skin disease called epidermolysis bullosa. These children have extremely fragile skin. These babies can have skin blisters form as a result of normal movement inside the uterus. Some of these blisters can be quite large, and sometimes, they may cause other anomalies, such as nose and ear problems, abnormal position of the first toe, bladder problems, and stiffness of the joints in the of the arms and legs.
Epidermolysis bullosa is a genetic disease. For a baby to have epidermolysis bullosa, it must have two copies of the abnormal epidermolysis bullosa gene. One abnormal gene copy is inherited from each parent, who are carriers for the disease (meaning they are healthy but have one normal gene and one abnormal gene).
Pyloric atresia can also be associated with hereditary multiple intestinal atresia. Babies with this problem can have blockages in any portion of intestinal tract, from the esophagus to the anus.
Should I have more tests done?
You will be offered additional testing to help determine the reason for the pyloric atresia. The exact testing offered will be based on the presence or absence of other ultrasound findings, your medical and pregnancy history, and your family history. You may also be offered a consultation with a Genetic Counselor, a medical professional with special training in genetic conditions.
Tests that may be offered include:
- A detailed ultrasound examination: This is to carefully look at your baby for any other ultrasound findings or abnormalities. Ultrasound can identify many but not all abnormalities.
- Amniocentesis: This is a test that removes a small amount of fluid from around the baby using a thin needle. The fluid can be tested for chromosomal abnormalities as well as fetal infections. Other genetic tests may be offered, such as chromosomal microarray (CMA, or “chip”) or Whole Exome Sequencing (WES) which look more closely at the genetic make-up of the fetus. These latter tests may not be readily available in all areas of the world.
What are the things to watch for during pregnancy?
Babies with pyloric atresia are at risk for polyhydramnios (too much amniotic fluid around the baby) and preterm labor during the pregnancy. Most specialists will recommend regular ultrasound examinations.
Polyhydramnios: If there is a blockage in the pylorus, amniotic fluid (water around the baby) cannot pass through to the duodenum where it is typically absorbed. This can cause an excess of amniotic fluid in the sac around the baby. Ultrasound examinations will help identify if too much amniotic fluid is accumulating around the baby. The presence of too much amniotic fluid is called polyhydramnios. You should alert your doctor or midwife if your abdomen feels tense or stretched or if you are short of breath or have trouble lying flat as this could be a sign of polyhydramnios.
Preterm labour: Polyhydramnios can stretch the uterus too much and cause early labour well before the due date. Knowing this in advance, your doctor or midwife can help with decreasing the risk of an early birth. Should you experience a sudden increase in the girth of your abdomen, frequent contractions, or a tense “balling up” of your abdomen, you should contact your doctor or midwife immediately.
What does it mean for my baby after it is born?
The biggest problem for babies with pyloric atresia is that they cannot digest swallowed fluid or milk. If these babies are fed, they will vomit to release the pressure in the stomach.
Babies who also have anomalies in other organs or a problem with their chromosomes may have even more problems after being born. The outcome for these babies depends on the type of problems that the baby has.
After birth, the baby will be admitted to the pediatric intensive care unit for evaluation and treatment. Additional imaging studies may be done to confirm the obstruction and to make sure the baby has no additional problems.
When the baby is stable, a surgeon will correct the obstruction and create a normal passage from the stomach through to the duodenum. The baby will stay in the intensive care unit in a specialized hospital for a few weeks after birth to recover from the surgery.
Babies with isolated pyloric atresia and no other structural differences, typically have no long-term problems.
Babies with pyloric atresia and epidermolysis bullosa, however, or with multiple intestinal atresias, unfortunately, have many problems and most die within the first few weeks of life.
Will it happen again?
When no genetic reason is found to explain the pyloric obstruction, the risk of this happening again is less than 1 in 100. If there is a genetic reason, then the risk depends on the genetic problem. Both epidermolysis bullosa and multiple intestinal atresia have a recurrence risk of 25%. Consultation with a specialist may be helpful.
What other questions should I ask?
- Does this look like a typical pyloric atresia?
- Are other anomalies (problems) identified?
- Should an amniocentesis be performed to look for chromosome anomalies?
- Is there a normal amount of amniotic fluid or is there too much fluid around the baby?
- How often will I have ultrasound examinations done?
- Where should I deliver?
- Where will the baby receive the best care after it is born?
- Can I meet in advance the team of doctors that will be looking after my baby when it is born?
Last updated October 2022
