This leaflet is to help you understand what Monochorionic Twins is, what tests you need and the implication of being diagnosed with Monochorionic Twins for you, your baby and your family.
What are monochorionic twins?
Monochorionic twins occur when one fertilized egg splits into two separate individuals with the same genetic makeup. These are considered identical twins. Monochorionic twins share the same chorion which is also known as the placenta.
Monochorionic twins are further classified based on whether or not the babies share the same amnion or amniotic sac. Monochorionic diamniotic (MCDA) twins share the same placenta but not the same amniotic sac and monochorionic monoamniotic (MCMA) twins share the placenta and amniotic sac.
How are monochorionic twins diagnosed?
Ultrasound (US) in the first trimester or early second trimester is the best time to diagnose monochorionic twins. At this time, your provider will also date the pregnancy and calculate your due date. Chorionicity, or the number of placentas present, is determined by using US to examine the membrane that projects off the placenta. The membrane in dichorionic twins is thicker and gives the appearance of a lambda and the membrane in monochorionic twins is much thinner giving the appearance of a “T.” Finding twins of different genders essentially rules out a monochorionic twin pregnancy.
What are the general complications of twin births?
Twins have an increased risk for birth defects or structural differences, preterm labor and being born early, growth differences, miscarriages, and stillbirth. There are other potential complications that can affect the babies after delivery. Moms of multifetal gestations are at increased risk of developing gestational diabetes, hypertensive disorders of pregnancy, anemia, cesarean delivery, postpartum hemorrhage, and postpartum depression.
What are the complications of monochorionic twins?
Complications unique to monochorionic pregnancies include twin-to-twin transfusion syndrome, twin anemia polycythemia sequence, and twin reversed arterial perfusion sequence. Umbilical cord entanglement and conjoined twins are risks unique to MCMA pregnancies.
What is twin-twin transfusion syndrome (TTTS) and how is it diagnosed and treated?
TTTS is an in-utero condition where one baby gets too much blood, while the other gets too little. It occurs in about 10-15% of twins that share the placenta. It is usually diagnosed by ultrasound evidence of a fluid imbalance between the two fetuses with one twin having an increase in the amount of amniotic fluid while the other has too little fluid. Depending on the severity, treatment can involve laser therapy of the placenta to stop the abnormal flow of blood from one twin to the other.
What is twin anemia polycythemia sequence (TAPS)?
TAPS occur in about 5% of MCDA pregnancies and is also caused by slow flow of blood from one fetus to the other through shared blood vessels within the placenta. This results in transfusion of blood from the donor twin to the recipient twin causing the donor to have low blood counts (anemia) and the other recipient twin to have high blood counts (polycythemia). It is diagnosed by using a Doppler ultrasound to look at the speed of blood flow within an artery (middle cerebral artery) in the fetuses’ brain. Management can vary based on severity but includes laser therapy or intrauterine blood transfusions.
What is twin reversed arterial perfusion sequence (TRAP)?
TRAP is a rare condition and occurs in about 1% of MCDA pregnancies. It results when the cardiac system of one twin does the work of supplying blood for both twins. The twin supplying the blood is known as the “pump twin” and develops normally. The other twin is known as the “acardiac twin” because it lacks a heart or has heart structures that are not fully formed. This twin mass has a poorly developed body and can be missing a head, limbs, and torso, resulting in severe anomalies that are incompatible with life. The structurally normal pump twin is at risk of heart failure due to continuous pumping of blood to the acardiac twin. Fetal surgery may be recommended to close off the blood vessels feeding the acardiac twin. Management varies and includes cord coagulation, cord ligation, photocoagulation of the anastomoses, or laser therapy.
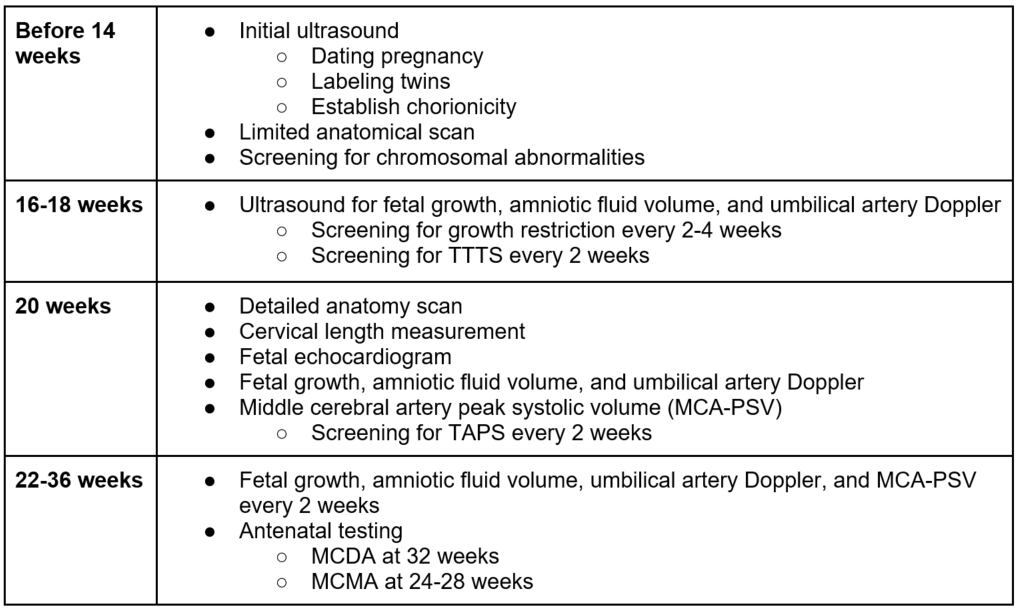
What type of surveillance or monitoring will I need?
When and how is it recommended that I deliver my babies?
It is recommended that uncomplicated MCDA twins are delivered at 36 weeks, and it is possible to deliver via vaginal birth if the presenting twin is head down. MCMA twins should be delivered between 32-34 weeks gestation by cesarean section due to ongoing risks of cord entanglement and potential fetal compromise.
What other questions should I ask?
- What is the chorionicity of my twin pregnancy?
- How often will I need to receive ultrasounds?
- Is there concern for any complications for my twins?
- When should I begin to receive closer fetal surveillance?
- When and where should I deliver?
- Can I have a vaginal delivery or is C-section recommended?
Last updated: September 2023
