Cervical ectopic pregnancy refers to an abnormal implantation of a fertilized ovum within the myometrium below the level of the internal os with a reported incidence of less than 1% of all ectopic pregnancies.
Cervical EP
Abstract: Cervical ectopic pregnancy refers to an abnormal implantation of a fertilized ovum within the myometrium below the level of the internal os with a reported incidence of less than 1% of all ectopic pregnancies. It can be classificated as partial or complete cervical pregnancy depending on whether the trophoblast is connected to the endocervical canal or not. Ultrasound is the primary diagnostic modality, Magnetic resonance imaging can be used as a second-line investigation if the diagnosis is equivocal. The most effective method of treatment for cervical pregnancy is yet to be found. Management options range from conservative therapies to surgical procedures. And often, more than one method is usually tried in the termination of cervical pregnancy.
Keywords: Cervical ectopic pregnancy, magnetic resonance imaging, ultrasound
Authors: Nguyen T Ha1, Lai T D Le1
-
Tu Du Maternal Hospital, Vietnam
Reviewers: Dr. Karen Fung Kee Fung
This article should be cited as: Lai Le, Nguyen Ha: Cervical Ectopic Pregnancy , Visual Encyclopedia of Ultrasound in Obstetrics and Gynecology, www.isuog.org, December 2021.
View the Patient Information leaflet
Definition
Cervical ectopic pregnancy refers to an abnormal implantation of a fertilized ovum within the myometrium below the level of the internal os [1].
ICD code
000.80
Incidence
The incidence of cervical pregnancy accounts for less than 1 percent of all ectopic pregnancies, estimated approximately 1 in 9000 pregnancies. It may be more common in pregnancies achieved through assisted reproductive technologies [2].
Pathogenesis
The etiology of cervical pregnancy is still unknown. There are a number of hypothesized causes of cervical pregnancy. Kouliev et al have hypothesized that the endometrium is damaged by a number of risk factors leading to the failure of blastocyst implantation. Studdiford postulated that rapidly transporting of a fertilized ovum through the endometrium caused a cervical implantation. Hofmann et al proposed that the endometrium is so immature for implantation. A prior history of curettage or local pathology related to previous cervical or uterine surgery may also be involved [2-5].
Classifications
True or primary cervical pregnancies are rare; cervico-isthmic and cervico-isthmic corporeal pregnancies are more common. True cervical pregnancies may occur more frequently than realized because they are aborted early without detection or disruption of the cervix, or may be confused with the cervical phase of a spontaneous abortion [5].
David MP et al (1980) classified as follows [2]:
1. Isthmico-cervical pregnancy: very low-lying placenta extending from above into the cervix
2. Pure cervical pregnancy: true cervical pregnancy limited to the first trimester, rarely reaching the second trimester
3. Cervico-isthmic pregnancy: transgression of a primary cervical pregnancy upward into the isthmus
4. Cervico-isthmic corporeal pregnancy: parts of the pregnancy invade the corpus
According to ESHRE (2019), cervical pregnancy can be classified as partial or complete depending on the presence or absence of their communication with the cervical canal. Complete cervical ectopics are completely confined to the cervical myometrium whereas partial cervical ectopics extend into the endocervical canal [1].
Risk factors
Any compromise in the capacity of the uterine cavity that prevents implantation in the endometrium could be a contributing factor. The major risk factors include in vitro fertilization, endometrial injury caused by pelvic inflammatory disease or postsurgical trauma such as Cesarean section or uterine curettage, history of abortions, intrauterine contraceptive device use, intrauterine adhesions, myomas, and structural uterine anomalies [6].
Recurrence risk
Recurrent cervical ectopic pregnancy is extremely rare. [8]
Diagnosis
In 1959, Palmann and Mc Elin proposed clinical criteria for a diagnosis of cervical pregnancy including [3,4]: (1) profuse but painless vaginal bleeding and amenorrhea, (2) a soft distended cervix that is usually larger than the corpus, (3) palpable placenta in the endocervix, and (4) a closed internal cervical os.
The most common symptom is vaginal bleeding. This clinical characteristic is named ‘painless vaginal bleeding’. However, it is not specific for cervical pregnancy. It must be distinguished from its mimickers like: cervical phase of spontaneous abortion, cervical cancer, cervical varicose veins, placenta previa, ruptured ectopic pregnancy, attempted illegal abortion, or choriocarcinoma [3]. Lower abdominal pain or cramps occur in fewer than one-third cases [2-5].
On speculum examination, the cervix is hyperemic, bulging and bluish discolored. In some cases, there are fetal membranes or pregnancy tissue at the external cervical os, which appear blue or purple. A cystic lesion on the cervical lip may be observed and represent trophoblastic invasion into the cervical stroma.
A suboptimal rise in serial human chorionic gonadotropin (ß-hCG) allows to suggest the diagnosis of an ectopic pregnancy but does not help to confirm the diagnosis of a cervical pregnancy [6].
Ultrasound is the primary diagnostic modality, using a transvaginal approach supplemented by transabdominal imaging if required. The following ultrasound criteria may be used for the diagnosis of cervical pregnancy [9]:
(1) An empty uterus
(2) A barrel -shaped cervix
(3) A gestational sac present below the level of the internal os
(4) The absence of the “sliding sign”,
(5) Blood flow around the gestational sac using colour Doppler.
Magnetic resonance imaging (MRI) can be used as a second-line investigation if the diagnosis is equivocal and there is local expertise in the MRI diagnosis of caesarean scar pregnancies [9]. The typical MRI finding of a cervical pregnancy is a heterogeneous hemorrhagic mass with densely enhancing papillary solid components [10].
Differential diagnosis
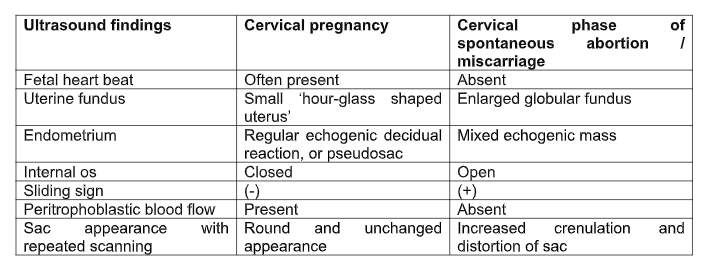
The main different diagnosis of cervical pregnancy is an ongoing miscarriage with a gestational sac passing through the cervix. The best way to distinguish the two situations is by the sliding sign. When gentle pressure is applied on the cervix with the probe, the implanted cervical pregnancy does not slide, unlike the gestational sac of the abortion. Furthermore, peritrophoblastic blood flow can be demonstrated on colour Doppler ultrasonography in case of cervical pregnancy. The visible fetal cardiac activity can also exclude an ongoing miscarriage. If there is any doubt as to whether a pregnancy is an ongoing miscarriage or a cervical pregnancy, repeat ultrasound is need to confirm the diagnosis.
Cervical pregnancy may be misdiagnosed as a Cesarean scar pregnancy. The difference is that cervical pregnancy is located below the internal os, while scar pregnancy is located above, at the level of the cesarean scar incision. All pregnancies implanted into the posterior cervix should be described as cervical pregnancies regardless of women’s previous history of delivery by Caesarean section. In cases of anterior implantation in women who have had a caesarean in the past, the differential diagnosis includes Caesarean scar ectopic pregnancy. In terms of management, they differ very little from Caesarean scar pregnancies [1]
Table 1. Differentiation of a cervical pregnancy from cervical phase of spontaneous abortion / miscarriage
Implication for ultrasound diagnosis
Cervical ectopic pregnancy is a rare and life-threatening condition. The incidence appears to be rising, not only due to assisted reproductive technologies, but also due to better access and accuracy of transvaginal ultrasound scanning. If there is a delay in diagnosis or treatment uncontrolled vaginal bleeding may result, leading to hysterectomy or even maternal death. Early diagnosis and treatment are the key to a successful outcome. However, accurate and timely diagnosis of cervical pregnancy is still a challenge because it can be mostly misdiagnosed as an ongoing abortion. This rare type of ectopic pregnancy, with its associated high risk of maternal morbidity and mortality should be suspected if the patient presents with the painless vaginal bleeding and a low implantation of gestational sac, under the internal os.
Prognosis
Ectopic pregnancy is still a significant source of maternal morbidity and mortality. Improved access to transvaginal ultrasound scanning facilities and the rapid assay of serum human chorionic gonadotropin (hCG) means that most ectopic pregnancies, including cervical pregnancies, are now diagnosed earlier. However, cervical pregnancy remains a high risk condition as it may present with a massive life-threatening hemorrhage secondary to the erosion of cervical blood vessels, and require emergency hysterectomy to minimize morbidity and mortality. Early diagnosis and management are the crucial steps for good outcome.
Management
Currently, the optimal method of treatment for cervical pregnancy is uncertain. Management options for cervical pregnancy range from conservative therapy to surgical procedures. Traditionally, cervical ectopic pregnancies have been managed surgically due to the anatomical location of cervical pregnancies. However, there has been a significant shift from such an approach to more conservative treatment modalities. Often, more than one method is employed to resolve cervical pregnancy.
Conservative management is either medical or expectant. Medical management may be systemic or intra-amniotic methotrexate administration, with or without intra-amniotic potassium chloride. To fulfill the criteria for conservative management, women have to be pain free, hemodynamically stable, pre-treatment serum β-HCG less than 5000 mUI/ml, absence of ultrasound evidence of fetal heart activity and patient’s agreement [6,8].
Curettage is the age-old fertility preserving method, but risks hemorrhage. Therefore, it has been used in conjunction with mechanical methods like cervical artery ligation and tamponade. Primary hysterectomy may still be the preferred treatment modality in cases of uncontrolled hemorrhage, second trimester or third trimester diagnosis of cervical pregnancy in an attempt to avoid emergency surgery and massive blood transfusion in a woman not desirous of fertility [13]
Arrest of bleeding can be achieved by tamponade of the uterine cervix with a Foley catheter, cervical cerclage, vaginal ligation of cervical arteries, uterine artery ligation, internal iliac artery ligation and angiographic embolization of the cervical, uterine or internal iliac arteries [11,13].
References
1. The ESHRE working group on Ectopic Pregnancy, Emma Kirk, Pim Ankum, Attila Jakab, Nathalie Le Clef, Artur Ludwin, Rachel Small, Tina Tellum, Mira Töyli, Thierry Van den Bosch, and Davor Jurkovic. Terminology for describing normally sited and ectopic pregnancies on ultrasound: ESHRE recommendations for good practice. Human Reproduction Open, Vol.00, No.0, pp. 1-21, 2020
2. David MP, Bergman A, Delighdish L. Cervico-isthmic pregnancy carried to term. Obstet Gynecol 1980;56:247–252.
3. Kouliev T, Cervenka K. Emergency ultrasound in cervical ectopic pregnancy. The Journal of Emergency Medicine, Vol.38, No.1, pp. 55–56, 2010
4. Hofmann HM, Urdl W, Hofler H, et al. Cervical pregnancy: case reports and current concepts in diagnosis and treatment. Arch Gynecol Obstet 1987;241:63–69.
5. Daniel M. Avery, Michael A. Wells, Diane M. Harper. Cervico-Isthmic Corporeal Pregnancy with Delivery at Term: A Review of the Literature with a case report. Obstetrical and Gynecological Survey, Vol 64, Issue 5, p. 335-344, May 2009
6. Vora PH, Jassawalla MJ, Bhalerao S, Nadkarni T: Cervical ectopic pregnancy: a clinician’s delemma. J Obstet Gynaecol India. 2016, 66:617-9.
7. Bouyer J, Coste J, Shojaei T, Pouly JL, Fernandez H, Gerbaud L, Job-Spira N. Risk factors for ectopic pregnancy: a comprehensive analysis based on a large case-control, population-based study in France. Am J Epidemiol. 2003 Feb 1;157(3):185-94
8. Christopher J. Radpour and Jeffrey A. Keenan. Consecutive cervical pregnancies. Fertiity and Sterility, Vol.81, No.1, January 2004
9. Diagnosis and Management of Ectopic Pregnancy, Green-top Guideline No. 21, 03 November 2016
10. Jung SE, Byun JY, Lee JM, Choi BG, Hahn ST. Characteristic MR findings of cervical pregnancy. J Magn Reson Imaging. 2001 Jun;13(6):918-22
11. Singh S. (2013). Diagnosis and management of cervical ectopic pregnancy. Journal of human reproductive sciences, 6(4), 273–276
12. C Sharma A, Ojha R, Mondal S, Chattopadhyay S, Sengupta P Niger, Cervical intramural pregnancy: Report of a rare case. Med J. 2013 Jul; 54(4):271-3.
13. Leeman LM, Wendland CL. Cervical ectopic pregnancy. Diagnosis with endovaginal ultrasound examination and successful treatment with methotrexate. Arch Fam Med. 2000;9:72–7.
Leave feedback or submit an image
We rely on your feedback to update and improve VISUOG. Please use the form below to submit any comments or feedback you have on this chapter.
If you have any images that you think would make a good addition to this chapter, please also submit them below - you will be fully credited for all images used.
Feedback form
Please note that the maximum upload size is 5MB, and larger images and video clips can be sent to [email protected].
