Heterotaxy is a wide spectrum of conditions characterized by an abnormal arrangement of thoracoabdominal organs across the left–right axis of the body.
Heterotaxy Syndromes
Abstract: Heterotaxy is a wide spectrum of conditions characterized by an abnormal arrangement of thoracoabdominal organs across the left–right axis of the body. It may be commonly referred to as isomerism, either right or left based, depending on which morphological structures are found on each side of the body. Heterotaxy syndrome is commonly associated with congenital heart disease, and may be associated with lung, spleen, liver, bowel, and biliary anomalies.
Keywords: Heterotaxy; atrial isomerism; situs inversus; congenital heart defect.
Authors: Roaa Gadeer1, Jane Lougheed2, Ana Werlang1
1. Department of Obstetrics and Gynaecology and Newborn Care, Division of Maternal-Fetal Medicine, The Ottawa Hospital, University of Ottawa, ON, Canada
2. Department of Pediatrics, Division of Pediatric Cardiology, The Children’s’ Hospital of Eastern Ontario, University of Ottawa, ON, Canada
Reviewers: Karen Fung-Kee-Fung
View the Patient Information leaflet
ICD code
ICD code: Q24
Definition
Heterotaxy is a wide spectrum of conditions characterized by an abnormal arrangement of thoracoabdominal organs across the left–right axis of the body. It differs from complete situs solitus and situs inversus(1). The word heterotaxy is derived from the Greek: ‘heteros’ meaning ‘other than’, and ‘taxis’ meaning ‘arrangement’. Therefore, heterotaxy, means a pattern of anatomical organization of the thoracic and the abdominal organs which is not the expected usual(2). Heterotaxy is also referred to as isomerism, which describes a situation in which right or left morphological structures are found on both sides of the body(1). The word isomerism is also derived from the Greek ‘iso’ meaning ‘equal’ and ‘meros’ meaning ‘part’. Isomerism refers to structures that are themselves in a mirror-image configuration (3).
Classification
The precise terminology of heterotaxy and the relationships of various disorders within heterotaxy syndrome are debated, but generally it is classified as follows:
1- Left atrial isomerism is associated with paired left-sided viscera while right-sided viscera may be absent. Left atrial isomerism accounts for most cases of “polysplenia syndrome”. Polysplenia is usually manifested as multiple splenic masses along the greater curvature of the stomach (4).
2- Right atrial isomerism is associated with paired right-sided viscera with absent or abnormal left-sided viscera. Right atrial isomerism is often associated with more severe and complex congenital heart disease and worse outcome as a result(5).
Both right and left isomerism have been described with the presence of a normal spleen and normal cardiac anatomy. Therefore, the presence or absence of spleen should not define the condition, but rather the mirroring of structures.
Incidence
Disorders of laterality and heterotaxy syndromes are rare diseases with an incidence of 1 - 1.5/10,000 live births(6). Heterotaxy syndrome, including right and left atrial isomerism, is found in between 2.2% and 4.2% of infants with congenital heart disease. The observed male-to-female ratio is 2:1(4).
Etiology and associations
1. Genetics:
• Most cases are sporadic.
• There is evidence to support multiple patterns of inheritance of heterotaxy. Heterotaxy occasionally occurs in a familial recurring pattern, suggestive of autosomal recessive, X-linked, or autosomal dominant inheritance.
• Familial heterotaxy is genetically heterogeneous with at least seven known heterotaxy genes (NODAL, ZIC3, CFC1, FOXH1, LEFTY2, GDF1, ACVR2B).
• Chromosome deletion/duplications or aneuploidy are uncommon causes(4).
• Ciliopathies: Heterotaxy may be associated with primary ciliary dyskinesia (PCD)(7,8).
2. Extracardiac involvement
• Malrotation.
• Biliary atresia (10% of left isomerism with interrupted IVC).
• Splenic dysfunction.
• Chronic lung disease.
Pathogenesis
During development there is a failure to form asymmetry along the left–right axis in the heterotaxy syndrome. In normal development, this asymmetry is first manifested at 2 to 23 days of gestation, with looping of the cardiac tube to the right. During this same period, abdominal situs is determined. The 270-degree counter clockwise rotation of the intestine about the axis of the superior mesenteric artery is completed by 10 weeks. The cardiac tube looping and intestinal rotation both occur during the 4th week of gestation, defects of cardiac situs are frequently associated with concomitant abnormal intestinal rotation. Heterotaxy is associated with congenital heart disease in the majority of cases because development of the heart is dependent on the formation of a normal left–right relationship (4).
Anatomical and sonographic features
Table 1:(4,5,8)
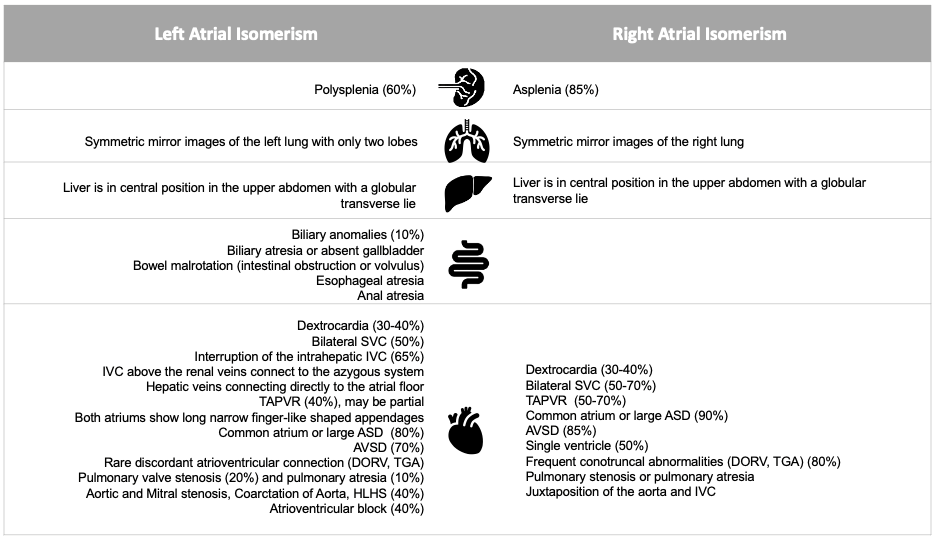
SVC: superior vena cava, IVC: inferior vena cava, TAPVR: total anomalous pulmonary venous return, ASD: atrial septal defect, AVSD: atrio-ventricular septal defect, DORV: double outlet right ventricle, TGA: transposition of great arteries, HLHS: hypoplastic left heart syndrome.
Recurrence risk
Most cases of heterotaxy are sporadic single occurrences. However, approximately 10% of cases have a family history of a close relative with congenital heart disease.
Recurrence of heterotaxy in families is not limited to the specific anomaly but may involve the full spectrum of heterotaxy, including right or left isomerism and situs inversus totalis(7).
Diagnosis
Suspicion of Heterotaxy syndrome on fetal ultrasonography is usually based on recognition of abnormal heart situs and/or abnormal arrangement of visceral organs.
Implications for sonographic screening and diagnosis
Antenatal diagnosis of heterotaxy syndrome is challenging and need an expert physician and sonographers.
The suspicion of Heterotaxy should be raised when the following exist:
• Dextrocardia is present.
• Heart and stomach situs are discordant.
• Complex congenital heart disease is present, especially in the presence of systemic or pulmonary vein abnormalities.
• Complete heart block associated with a congenital heart defect.
• The liver is large and midline(8).
Heterotaxy can be associated with wide range of congenital heart disease and systematic defects but there are some lesions associated more with RAI or LAI. (See Table 1).
Evaluation of suspected cases of heterotaxy syndrome should start with:
• Assessment of situs (fetal position, heart and stomach to the left).
• Four chambers view (identification of normal septal view to rule out possible atrioventricular septal defects; assessment of pulmonary veins and relationship to atria; morphological appearance of atria and ventricles).
• Assessment of outflow tracts and relationship of great arteries (sweep superiorly through the level of four chambers view to reveal the outflow tracts).
• Three vessel view (persistent left superior vena cava (LSVC) can be seen as fourth vessel in this view).
• Evaluate Venous anatomy (normal bicaval view, makes the diagnosis of interrupted inferior vena cava less likely but does not eliminate the possibility of bilateral SVC).
• Look carefully for prominent vessel running parallel to descending aorta which may indicate the presence of interrupted IVC with azygous continuation.
(The azygous vein will be large, prominent as the descending aorta and runs parallel to it, can be appreciated as “double vessel “sign at the level of the four-chamber view. Colour Doppler can display parallel vessels with opposite direction of flow in the midsagittal view).
• Assessment of the cardiac rhythm (to rule out fetal bradycardia often associated with heterotaxy syndrome)(7,9).
“Refer to Power Point images for illustration.
“See ISUOG Practice Guidelines (updated): sonographic screening examination of the fetal heart”.
Role of Fetal MRI in Heterotaxy syndrome
A high-level ultrasound which is done by highly trained and skilled fetal imager is the keystone to diagnosis of heterotaxy syndrome. Fetal MRI may have a role in selected cases in assessing bronchial morphology, spleen presence or absence and the number of splenic masses. Furthermore, it permits the assessment of intestinal obstructions/ malrotation(9).
The use of fetal MRI is not widely used due to the high cost of the test, accessibility issues in some centers, and the need for fetal MRI imaging expertise.
Prognosis
The prognosis depends largely on the type and severity of the associated cardiac malformations. The current survival rate has improved due to increased prenatal detection, early referral to highly specialized centers and improvements in surgical intervention. Poor prognostic risk factors include cases with obstructed anomalous pulmonary venous return, complete heart block, significant atrioventricular valve regurgitation, and single ventricle anatomy. Patients with LAI in general have less severe cardiac malformations than those with RAI and thus better outcomes including higher chance of biventricular repair. Many patients with RAI and some with LAI will follow a single ventricle palliation pathway with a Fontan-type repair(3,8).
Although neonatal morbidity and mortality are determined mainly by the congenital heart defects, varying degrees of malrotation of the bowel, gastric volvulus, biliary atresia and immune system dysfunction associated with splenic anomalies significantly influence long-term survival in children with heterotaxy syndrome(5).
Multidisciplinary management
Prenatal Consultation with:
• High-risk obstetrician for pregnancy and delivery management.
• Neonatology.
• Pediatric Cardiology.
• Genetics, especially if a positive family history of heterotaxy or congenital heart disease.
Fetal Follow-up:
• Regular assessment of fetal growth and well-being, including assessment for fetal hydrops.
• Repeat pediatric echocardiography to reassess for progression in atrioventricular valve regurgitation, outflow tract obstruction, ventricular hypoplasia, complete heart block.
• Consider delivery in a tertiary care facility. Emergent or urgent neonatal cardiac surgery may be required, so delivery is recommended to occur at or near a congenital cardiac surgical centre.
• Prostaglandin E infusion may be needed at delivery for ductal dependent congenital heart defects(8–10).
Prevention
Excellent glycemic control prior to planning pregnancy is recommended in diabetics. Drugs used in nicotine dependence treatment, cocaine use in the first trimester and opiate exposure (heroin and methadone) should be avoided(11).
References
1. Buca DIP, Khalil A, Rizzo G, Familiari A, di Giovanni S, Liberati M, et al. Outcome of prenatally diagnosed fetal heterotaxy: systematic review and meta-analysis. Vol. 51, Ultrasound in Obstetrics and Gynecology. John Wiley and Sons Ltd; 2018. p. 323–30.
2. Jacobs JP, Anderson RH, Weinberg PM, Walters HL, Tchervenkov CI, del Duca D, et al. The nomenclature, definition and classification of cardiac structures in the setting of heterotaxy. In: Cardiology in the Young. 2007. p. 1–28.
3. Kim SJ. Heterotaxy syndrome. Vol. 41, Korean Circulation Journal. Korean Society of Cardiology; 2011. p. 227–32.
4. Bianci DW, Crombleholme TM, Dalton ME, Malone FD. Fetology: diagnosis and management of the fetal patient . 2nd ed. McGraw- Hill; 2010.
5. Gottschalk I, Stressig R, Ritgen J, Herberg U, Breuer J, Vorndamme A, et al. Extracardiac anomalies in prenatally diagnosed heterotaxy syndrome. Ultrasound in Obstetrics and Gynecology. 2016 Apr 1;47(4):443–9.
6. Gottschalk I. Disorders of Laterality and Heterotaxy in the Foetus. 2012;216(3).
7. Abuhamad AZ CR. A Practical Guide to Fetal Echocardiography . 3rd ed. 2012.
8. Woodward PJ, Kennedy A, Sohaey R. Diagnostic Imaging . Elsevier Health Science ; 2016.
9. Degenhardt K, Rychik J. Fetal Situs, Isomerism, Heterotaxy Syndrome: Diagnostic Evaluation and Implication for Postnatal Management. Vol. 18, Current Treatment Options in Cardiovascular Medicine. Springer Healthcare; 2016.
10. Akalın M, Demirci O, Kumru P, Yücel İK. Heterotaxy syndrome: Prenatal diagnosis, concomitant malformations and outcomes. Prenat Diagn. 2022 Apr 1;42(4):435–46.
11. van Veenendaal NR, Kusters CDJ, Oostra RJ, Bergman JEH, Cobben JM. When the right (Drug) should be left: Prenatal drug exposure and heterotaxy syndrome. Birth Defects Res A Clin Mol Teratol. 2016 Jul 1;106(7):573–9.
This article should be cited as: Gadeer R, Lougheed J, Werlang A: Heterotaxy syndrome, Visual Encyclopedia of Ultrasound in Obstetrics and Gynecology, www.isuog.org, April 2023.
Leave feedback or submit an image
We rely on your feedback to update and improve VISUOG. Please use the form below to submit any comments or feedback you have on this chapter.
If you have any images that you think would make a good addition to this chapter, please also submit them below - you will be fully credited for all images used.
Feedback form
Please note that the maximum upload size is 5MB, and larger images and video clips can be sent to [email protected].
